Surgical Revenue cycle Management
Accelerate growth.
Leverage intelligent analytics.
Achieve powerful financial results.
Join more than 1,100 surgical organizations who trust nimble’s platform and advisors to bring deep insights and actionable intelligence to maximize their revenue cycle.
1,100+
surgical clients
$10 billion+
in net collections
25 million+
charts coded
Our surgical revenue cycle management expertise, your advantage.
Over the past 20 years, clients have trusted nimble to manage over $10 billion in net revenue. See how the industry’s most comprehensive suite of surgical RCM solutions will streamline and strengthen your business.
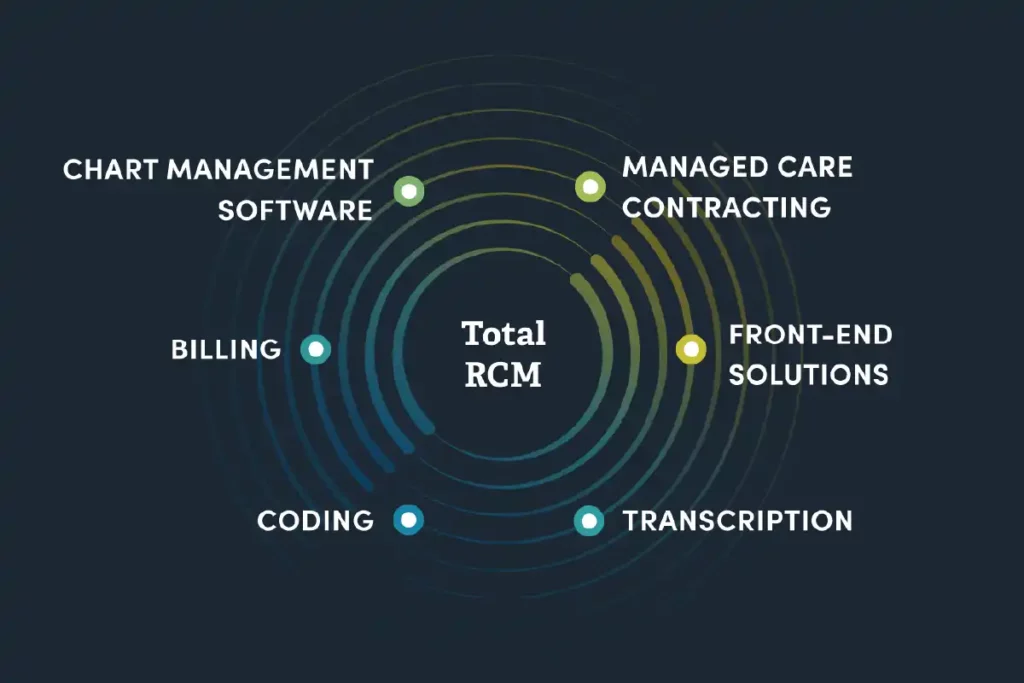
Maximize revenue, get paid faster, and stay compliant with the industry’s most powerful surgical revenue cycle management solution.
Ensure maximum reimbursement for every procedure by leveraging our team’s unparalleled knowledge and expertise.
Ease your administrative burden while reducing payer denials with our integrated suite of front-end solutions, including patient demographics, pre-authorization, patient estimates, and scheduling and credentialing tools.
Build new efficiencies to improve the speed and accuracy of your transcription process, with a fully integrated web-based management tool, easy-to-use mobile app, and around-the-clock support.
Access the best and most experienced team of surgical coders to expedite reimbursement with 24-hour turn-around-times and accurate, compliant coding, all delivered through our comprehensive management tool and interactive dashboard.